This article by Bill Sullivan, Indiana University School of Medicine originally appeared on the Conversation and is published here with permission.
Albert Alexander was dying. World War II was raging, and this police officer of the county of Oxford, England, had developed a severe case of sepsis after a cut on his face became badly infected. His blood was now teeming with deadly bacteria.
According to his physician, Charles Fletcher, Alexander was in tremendous pain, “desperately and pathetically ill.” The bacterial infection was eating him alive: He’d already lost one eye and had oozing abscesses all over his face and in his lungs.
Since all known treatment options were exhausted and death appeared imminent, Fletcher decided that Alexander was the perfect candidate to try a new, experimental therapy. On Feb. 12, 1941, Alexander became the first known person to be treated with penicillin. Within days he began to make a stunning recovery.
I am a professor of pharmacology, and Alexander’s story is the prelude to my yearly lecture on antibiotics. Like many other microbiology instructors, I’d always told students that Alexander’s septicemia arose after he scratched his cheek on a thorn while pruning rosebushes. This popular account dominates the scientific literature as well as recent articles and books.
The problem is, while descriptions of the miraculous effect of penicillin in this case are accurate, the details of Alexander’s injury were muddled, likely by wartime propaganda.
Breaking the mold
The promise of penicillin as an antibiotic was first noted in 1928, when microbiologist Alexander Fleming noticed something funny in his petri dishes at St. Mary’s Hospital in London. Fleming’s cultures of staphylococcal bacteria did not grow well on plates contaminated with a penicillium mold. Fleming discovered that the mold’s “juice” was lethal to some types of bacteria.
A decade later, a team of scientists led by Howard Florey at Oxford University began the arduous task of purifying the active substance from the “mold juice” and formally testing its antimicrobial properties. In August 1940, Florey and his colleagues published their striking findings that purified penicillin safely wiped out numerous bacterial infections in mice.
Florey then sought Fletcher’s help to try penicillin in a human patient. That patient would be Alexander, whose death seemed inevitable otherwise. As Fletcher stated, “There was all to gain for him in a trial of penicillin and nothing to lose.”
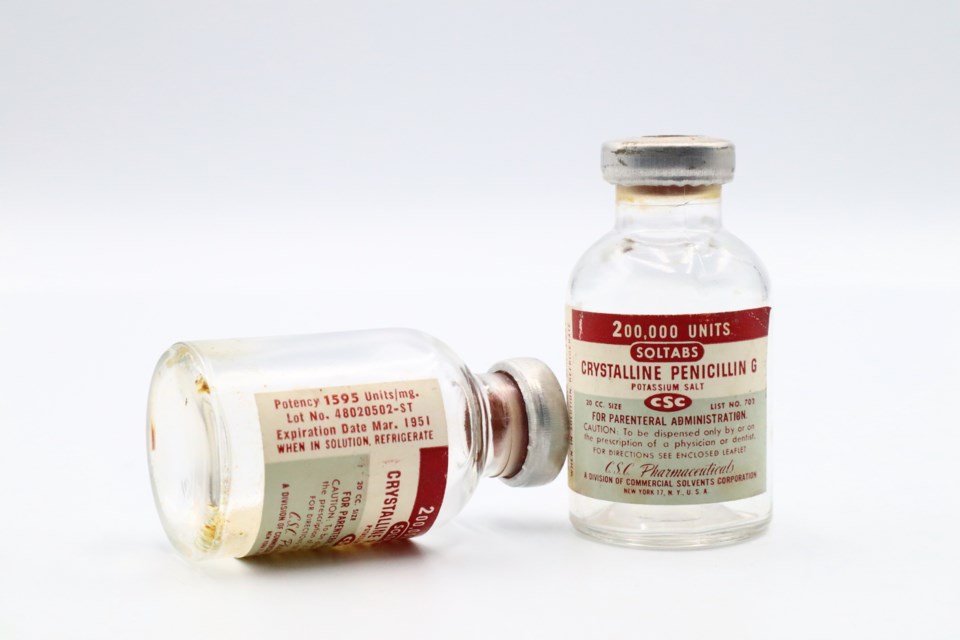
At the time, purified penicillin was extremely scarce, since the mold was slow to grow and yielded precious little of the drug. Despite recycling unprocessed penicillin from Alexander’s urine, there just wasn’t enough available to finish off the infection once and for all. After 10 days of improvement, Alexander gradually relapsed. He died on March 15, 1941, at the age of 43.
Despite the tragic outcome, Alexander’s case turbocharged interest in penicillin research. As Fletcher observed, “There was no doubt about the temporary clinical improvement, and, most importantly, there had been no sort of toxic effect during the five days of continuous administration of penicillin.”
Almost exactly a year later, on March 14, 1942, doctors in Connecticut administered the antibiotic to a woman named Anne Miller who was deathly ill with streptococcal septicemia. She made a full recovery and became the first patient cured with penicillin. Mass production of penicillin became a top priority of the U.S. War Department, second only to the Manhattan Project. It is widely believed that penicillin helped the Allies during World War II, preventing wound infections and helping soldiers diagnosed with gonorrhea to return to the battlefield.
The rosebush tale has been a thorn in their sides
Albert Alexander has earned a place in history as the first known person to be treated with penicillin for a clinical condition. Almost as famous as his name is the purported cause of death: sepsis due to a scratch from rosebushes.
However, an alternative explanation was revealed in a 2010 interview with Eric Sidebottom, a historian and author of “Oxford Medicine: A Walk Through Nine Centuries.” He claimed that Alexander was injured when his police station was hit during a German bombing raid on Nov. 30, 1940. Shrapnel from this attack caused the facial lacerations that led to Alexander’s fatal blood poisoning, he said.
Alexander’s daughter, Sheila LeBlanc, who moved to California and became an artist, confirmed Sidebottom’s account in a 2012 interview with a local newspaper. She also revealed the grim consequences Alexander’s death had on his family. Since they’d lived in a house provided by the village, for the village constable, his death forced them to move out. LeBlanc, who was seven at the time, and her older brother were sent to an orphanage, since their mother had to find work.
Michael Barrett, a professor of biochemical parasitology at the University of Glasgow, also spoke to LeBlanc about the cause of Alexander’s injury. Writing in 2018, Barrett stated that while LeBlanc recalled that the constable’s house did have a beautiful rose garden, her father’s fatal cut was sustained during the German blitz.
In February 2022, I contacted Alexander’s granddaughter, Linda Willason, who is also an artist in California, to help set the record straight. Willason validated the shrapnel account and suggested that the rosebush story was “a bit of wartime propaganda.” By downplaying bombing injuries, the government likely hoped to maintain the public’s stiff upper lip.
While the nature of Alexander’s injury may seem a trivial detail, correcting the historical record is important. Alexander died in the line of duty, and the apocryphal rosebush story obscures his honorable actions. His descendants are hopeful the true account of his injury will now eclipse the false one.
In 2021, a plaque commemorating Alexander was installed in Newbury that reads: “On war support duty in Southampton on 30th November 1940, Albert was injured in an air raid. Contracting staphylococcal and streptococcal septicaemia, he was transferred to the Radcliffe Infirmary in Oxford, where he was selected for the first clinical application of penicillin. … His place in the history of antibiotics is secure.”
[You’re smart and curious about the world. So are The Conversation’s authors and editors. You can read us daily by subscribing to our newsletter.]
Bill Sullivan, Professor of Pharmacology & Toxicology, Indiana University School of Medicine
This article is republished from The Conversation under a Creative Commons license. Read the original article.